Lung-substitute medical devices in the news, including Injectable Oxygen, and, an Overview of Drawbacks of Many Current Artificial Oxygenating Methods
You may also be interested in another page on this website:
“Artificial Lungs in the News”
In the news on this date (November 23, 2009) was a swine flu-related story of how an alternative oxygenating method, ECMO (extracorporeal membrane oxygenation), was being successfully used to allow patients whose lungs were temporarily compromised from their illness to “breathe” mechanically in the interim.
From the AP (headline is link):
Trying Last-Ditch Lung Bypass For Worst Swine Flu
WASHINGTON – A technology originally developed for premature babies may be helping to save some of the sickest swine flu patients by rerouting their blood so their lungs can rest.
It’s a risky approach using equipment that only certain specialized hospitals have. But faced with children and young adults struggling to breathe despite ventilators has intensive-care doctors dusting off these machines, named ECMO, that they often consider last-ditch and almost never use for influenza.
“It was pretty scary knowing that was his blood flowing through those tubes in and out of his body,” says Susie Damm of Omaha, Neb., whose 19-year-old son Ryan survived a life-threatening bout after 10 days on ECMO.
“I was one of the people sick and tired of hearing about the swine flu, thinking people were making a big deal of it,” she adds. “Now I’ve had a different look, and I’m very, very thankful” he survived.
No one knows which patients are most likely to benefit — not everyone does. But ECMO is gaining attention after Australian researchers reported that the machines helped during that country’s outbreak of what scientists call the 2009 H1N1 flu strain. A voluntary U.S.-based registry counts 107 critically ill swine flu patients recently treated with ECMO, most from this country.
In Omaha, Dr. Jeff DeMare credits the technique with saving Ryan Damm and 7-year-old Tania Romero-Oropeza after both patients’ lungs went from clogged to nearly useless in a stunning matter of hours. Tania’s care was complicated by a drug-resistant staph infection.
“You wonder, ‘OK, we’ve got a lot of folks who get this disease and why is it so bad in some cases?’ We don’t have a real good handle on that,” says DeMare, a critical care specialist at Children’s Hospital & Medical Center.
Whatever the reason, “your body needs time to fight the infection,” he adds, and he gambled that the pricey equipment could buy that time.
Estimates from the federal Centers for Disease Control and Prevention suggest that swine flu has hospitalized 98,000 Americans in the past six months, and killed nearly 4,000. For most, standard treatment works.
But the sickest often need ventilators to pump their lungs, and ventilators damage lung tissue, especially as they’re turned up to higher pressures as patients worsen.
Hospitals are “exhausting all measures” on those patients, says Dr. Pauline Park, a University of Michigan ICU co-director who’s helping to analyze the ECMO registry in hopes of determining best candidates. “Physicians don’t want to give false hope to families, but also don’t want to stand by if a life can be saved.”
Enter ECMO, decades-old technology that essentially offers a temporary lung bypass. Tubes carry blood out of the body so a filter can remove carbon dioxide and reinfuse oxygen, and then dump the blood back.
It’s a twist on the heart-lung machine used for open-heart surgery, modified so that patients can stay on the machine for weeks instead of just hours and, key here, so that blood doesn’t have to bypass the heart if only the lungs need a rest.
There are many cautions. It’s risky, requiring blood thinners to avoid clots and posing the potential for additional infection. It can double the cost of ICU care. Only about 120 hospitals in the U.S. offer it, most just a few times a year for newborns with respiratory failure, its primary use.
ECMO in adults is hugely controversial because past research couldn’t prove that it significantly increased survival.
Here’s what’s new:
Australian researchers reported last month that they used ECMO in 68 critically ill swine flu patients who failed standard care, and about 71 percent survived. That research predicted some 800 people might be ECMO candidates if the U.S. experienced similar rates of swine flu.
Coincidentally, a British study also published last month found that nearly two-thirds of adults randomly assigned to ECMO survived other types of respiratory failure — before swine flu hit — while just 47 percent survived with regular ICU care. It’s the most rigorous study of ECMO performed in adults and one that has lung specialists debating wider use.
Preliminary data from the Michigan-run ECMO registry suggests survival can reach 72 percent if recipients get it within six days of using a ventilator. With longer ventilator use, the survival rate plummets.
Back in Omaha, DeMare agrees ECMO shouldn’t be last-ditch, noting his own patients were on ventilators for just hours before getting it. Still, Tania had a monthlong hospital stay, including her eight days on ECMO.
“Thank God the doctor took that decision to use this machine,” said Tania’s mother, Antonieta Oropeza, speaking in Spanish through an interpreter.
Additional in-depth information on ECMO/ECLS (extracorporeal life support) is at this following site, among others, though it is geared toward the use of it for infants and discusses at length the drawbacks encountered in a number of such cases. The image below is from a previous version of that article.
http://seattletimes.nwsource.com/html/health/2010337795_apusmedhealthbeatflulungmachine.html
The relevant patent numbers for this type of invention are:
-Extracorporeal Blood Processing System U.S. Patent # 4599093
-Extracorporeal Circulation Apparatus U.S. Patent # 4828543
The patent abstract for the second number above has in it an instructive overview on the workings of the body’s circulatory and oxygenating systems, worthwhile enough to bear duplicating here for general information.
“The present invention relates generally to the field of extracorporeal circulation of bodily fluids. More particularly, it relates to circulation and processing of blood outside the body. Still more particularly, it relates to regulating the rates and pressures of blood flowing through an extracorporeal processing circuit.
The human body is a complicated organism. It carries out a myriad of functions and processes around the clock, day-in and day-out. Sometimes the body is unable to perform vital tasks completely or adequately. Circumstances sometimes require medical treatment to assist or replace bodily functions. Medical science has devised various machines and equipment to help the systems of the body meet the demands placed on them in ordinary and extraordinary situations. One system extremely crucial to proper operation of the body is the cardiovascular system.
The cardiovascular system includes the heart and all the blood vessels in the body. The heart provides force to pump blood through the system. The arterial system connects to the heart and fans out in increasingly smaller vessels to the far reaches of the body, linking ultimately to capillaries. Capillaries are the smallest vessels in the cardiovascular system. Capillaries form minute networks throughout the body’s tissues. The capillaries eventually connect to veins. Veins, constituting the venous system, lead finally back to the heart.
Blood is a highly complex fluid. It contains, generally, plasma and cells. The cell component comprises red blood cells, white cells, and platelets. Plasma is mostly water with a tremendous variety of solutes. These solutes include inorganic components, metaboli nutrients and byproducts, and a host of plasma proteins.
Blood flows from the heart to the arteries, then to the capillary network. The blood brings nutrients and oxygen to the cells of the body. All cells need these substances to live. The blood also gathers carbon dioxide and other waste products resulting from the body’s matabolism. These wastes must be removed to allow cells to continue functioning. The returning blood collects in the veins and flows back to the heart. This returning blood carries the collected waste. The kidneys treat the blood to remove such waste products. These wastes, if left in the blood, would ultimately be fatal. Kidneys perform the vital function of cleansing the blood. Lungs likewise help to rejuvenate the blood. The major function of the blood’s red cells is to transport oxygen from the lungs to body tissues and to help transport carbon dioxide from the tissues back to the lungs. The heart pumps returning venous blood to the lungs. The lungs contain semipermeable membrane tissue that allows gases to migrate across it. Carbon dioxide passes from the blood into the lungs to be exhaled, while oxygen in the lungs is absorbed by the red blood cells. This newly oxygenated blood then returns to the heart for subsequent re-circulation through the cardiovascular system.
The process of circulating, cleansing, and oxygenating of the blood, then, is essential to life. The natural mechanical and biochemical systems of the body, when operating properly, perform these tasks best. Sometimes, though, a medical patient’s condition prevents proper functioning of the blood system. The ability to supplement or replace the blood system then becomes crucial to the patient’s survival.
Existing extracorporeal circulation apparatus for treating blood generally remove and collect a patient’s whole blood, circulate the blood through an extracorporeal circuit, and return the treated blood to the patient. Depending on the specific application, the treating involves filtering, removing some component(s) from the blood, or oxygenation. Various techniques and apparatus have been used in different blood treatment applications.Heart-lung machines used during surgery pump and oxygenate blood, in place of a patient’s heart and lungs. Existing oxygenators suffer from imprecise control and inefficient operation. Blood flows through semi-permeable hollow fibers or channels inside semi-permeable membranes. Utilizing at least one pump in series with the oxygenator, the blood is pressured sufficiently to flow in the form of thin film layers along the membrane walls, thereby maximizing the flowing surface area. The partial pressure of oxygen on the exterior of the membrane walls is kept sufficiently high for the red cells of the venous blood to absorb the oxygen; similarly, the partial pressure of carbon dioxide on the membrane exterior is low enough to allow the venous red cells to discharge carbon dioxide. Oxygen on the membrane exterior migrates across the membrane for absorption by the blood, and carbon dioxide exits the blood and migrates to the membrane exterior. Inadequate control of the transmembrane pressure, however, often requires recirculation of the blood through the circuit after initial oxygenation. What pressure control exists is merely regulation of pump speeds as an indirect, and inaccurate, means for maintaining hoped-for pressure differnentials. There is no true, direct control of oxygenation based on transmembrane pressure. Instead, direct observation of blood colors and pressures ordinarily helps ascertain if blood leaving the system has been properly oxygenated. Such crude operational methods demonstrate the need for improved, effective, efficient control of blood oxygenating apparatus. It is apparent that extracorporeal circulation and treatment of blood is a necessary, vital process for a wide range of medical treatments. Known apparatus for performing this process have suffered from numerous inefficiencies, operational problems, inadequate regulation, and economic disadvantages. A serious need has existed for an efficient, simple, controllable, yet economical means for circulating and treating blood outside the human body.”
Now Comes… Injectable Oxygen
Acknowledging the information above on the need to remove waste buildups in the blood of components such as carbon dioxide, there is another technology announced in 2012 (only brought to attention here in 2016) that is yet one more way of bypassing the lungs: Injectable Oxygen.
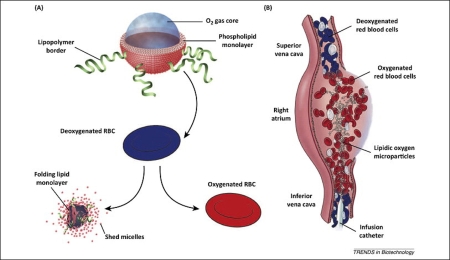
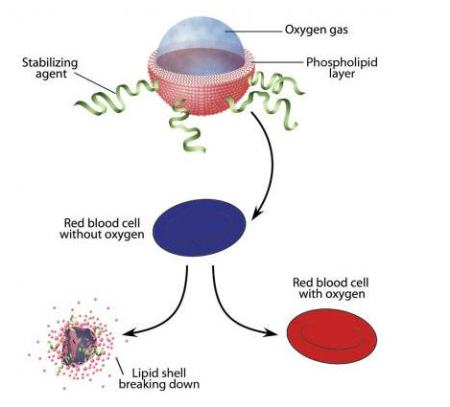
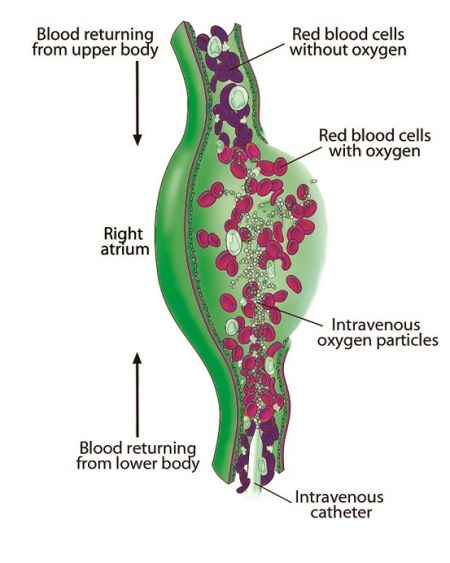
“A team led by researchers at Boston Children’s Hospital has designed tiny, gas-filled microparticles that can be injected directly into the bloodstream to quickly oxygenate the blood. The microparticles consist of a single layer of lipids (fatty molecules) that surround a tiny pocket of oxygen gas, and are delivered in a liquid solution. The microparticles would likely only be administered for a short time, between 15 and 30 minutes, because they are carried in fluid that would overload the blood if used for longer periods.”
Will this, perhaps, be the technology that gets us over the hump of bypassing the lungs for consciousness exploration?
Listen to the doctor who is the inventor of this method discuss his technique with an interviewer: https://wordpress.com/page/mergenthalerlinotype.wordpress.com/554
(two more separate, slightly different versions of the previous graphic presented below)

November 29, 2010 at 10:50 pm |
In the realm of natural breathing difficulties, I should mention a relatively new, simple, low-cost device that apparently does wonders for people with conditions ranging from simple “clearing the throat/lungs” in the morning to Chronic Obstructive Pulmonary Disease (COPD; typically brought about by smoking*.)
It goes by the odd moniker of Lung Flute. This innocuous-looking breakthrough, one of Popular Science magazine’s 100 best inventions of 2009 (http://www.popsci.com/bown/2009/product/medical-acoustics-lung-flute), helps a person that is in not so bad of shape as to need ECMO to more easily breathe for being able to clear the lungs in a manner not achieved by other methods.
The basic concept is to stimulate the cilia in the lungs to do their job more effectively; this stimulation from a sympathetic induced vibration geared to the cilia’s natural rate of around 15 cycles per second. You could visualize this as the Pied Piper blowing a mean riff on said Lung Flute and getting all the cilia to dance in tune with him.
Obviously my fanciful prose lacks a bit…. Here are the links you would get if you searched the term and from therein you can be more effectively enlightened:
http://medicalacoustics.com/
http://copd.about.com/od/copdtreatment/fr/lungflutereview.htm
*COPD is one of the most common lung diseases. It makes it difficult to breathe. There are two main forms of COPD:
– Chronic bronchitis, defined by a long-term cough with mucus
– Emphysema, defined by destruction of the lungs over time